
Posted By: Medsole RCM
Posted Date: Feb 19, 2026
You've just brought a new physician on board. They're qualified, eager to see patients, and ready to generate revenue for your practice. But there's a problem. Without proper credentialing, every single claim they submit will be denied. The insurance company won't pay a dime until that provider is verified, enrolled, and listed as in-network. And the average timeline to get through this process? Somewhere between 90 and 120 days. That's up to four months where a fully capable doctor can't earn your practice a cent from insured patients.
The financial damage adds up fast. A physician seeing 20 patients a day at an average reimbursement of $150 per visit loses your practice roughly $3,000 every single day they aren't credentialed. Over 90 days, that's $270,000 in revenue you'll never recover. And that doesn't account for the patients who simply go elsewhere because you're listed as out-of-network.
This guide breaks down everything you need to know about physician credentialing services and medical credentialing services in 2026. You'll learn how the process actually works step by step, what it should cost (and what most companies won't tell you about pricing), which new CMS and NCQA rules took effect this year, and how to evaluate credentialing services so you pick the right partner the first time.
At MedSole RCM, we handle provider enrollment and credentialing services as part of our full revenue cycle management solution. Our pricing is $99 per provider, flat rate, no hidden fees. We complete credentialing in 45 to 60 days across all 50 states. We publish that number because we believe you deserve to know what you'll pay before you ever pick up the phone.
Physician credentialing is the formal process of verifying a healthcare provider's qualifications before they can treat patients and bill insurance. Think of it as the background check that stands between a doctor and their ability to get paid.
During credentialing, insurance companies, hospitals, and regulatory bodies verify specific details about a provider. These include medical school education, residency and fellowship training, active state medical licenses, DEA registration, board certification status, malpractice insurance coverage, and work history. Every piece of documentation gets checked against its original source, a process called primary source verification, or PSV.
This verification isn't optional. NCQA credentialing standards require it. The Joint Commission mandates it for hospital privileges. And CMS provider enrollment requirements make it a prerequisite for Medicare and Medicaid participation. Without completing this process, a provider simply cannot participate as an in-network physician with any insurance payer.
The credentialing meaning in healthcare goes beyond simple background checks. Medical credentialing confirms that a provider meets every standard required by the specific payer, facility, or regulatory body they want to work with. Each payer sets its own criteria. Each state has its own licensing requirements. And each facility may add additional privileging requirements on top of everything else.
Once credentialing is complete, the provider receives an effective date from each payer. That date marks when they can finally begin submitting claims as an in-network provider. Everything before that date? Either denied or reimbursed at significantly lower out-of-network rates.
The business case is straightforward. No credentialing means no in-network billing. No in-network billing means no insurance reimbursement at contracted rates.
Patients actively avoid out-of-network providers. Their copays are higher, their deductibles are larger, and their insurance covers less. When a provider isn't credentialed, most insured patients will choose someone who is. That means fewer appointments, lower collections, and a shrinking patient panel.
Credentialing in healthcare also satisfies compliance requirements that protect both the practice and its patients. Payers need assurance that every provider in their network meets minimum quality and safety standards. Hospitals need documentation that a physician is qualified to perform specific procedures within their facility.
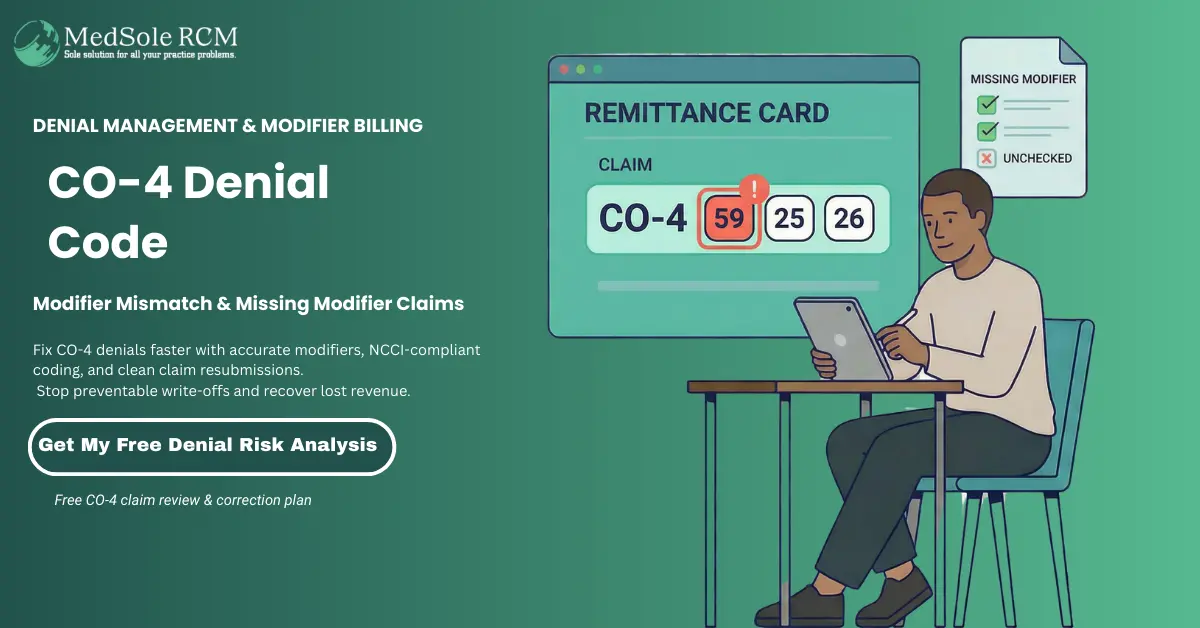
Beyond compliance, credentialing directly affects claim acceptance. A provider's NPI number must be linked to active payer enrollments. If that link doesn't exist, claims bounce. Denied claims create accounts receivable backlogs, increase administrative work, and delay cash flow. For practices already managing tight margins, that's a problem that compounds every week it goes unresolved.
Here's what most providers don't realize until it's too late: credentialing isn't an administrative task. It's a revenue event. Every day a provider sits uncredentialed is a day your practice bleeds money.
Let's do the math. A single physician generating 20 patient visits per day at an average reimbursement of $150 per visit produces $3,000 in daily revenue. Over a standard 90-day credentialing timeline, that's $270,000 in potential collections sitting on the table. For a group practice onboarding three new providers simultaneously, the exposure climbs to over $800,000.
And the losses don't stop at missed visits. When credentialing is delayed or incomplete, the ripple effects hit your entire revenue cycle. Claims submitted before the effective date get denied. Your billing team spends hours working claim denials and revenue loss that should never have occurred. Your revenue cycle management metrics deteriorate: days in AR climb, denial rates spike, and net collection percentages drop.
The worst part? Commercial payers don't allow retroactive billing in most cases. Once that effective date passes, there's no going back to capture revenue from the gap period. The money is gone. Your AR follow-up team can chase every other outstanding dollar, but they can't recover revenue that was never billable in the first place.
The industry standard timeline of 90 to 120 days isn't a fixed number. It's an average. Some payers move faster. Others drag things out well past 150 days, especially for certain specialties or in states with complex regulatory requirements.
During that waiting period, your practice faces a choice. Either the new provider sees no insured patients at all, or they see patients and the practice bills at out-of-network rates. Both options hurt. Out-of-network billing means lower reimbursement, higher patient responsibility, more balance billing disputes, and a reputation hit when patients see larger-than-expected bills.
What extends these timelines even further is preventable errors. An expired license on the application. A gap in the CV that wasn't explained. A CAQH profile that lapsed because nobody re-attested it within the required 120-day window. Each mistake triggers a rejection, and each rejection restarts the clock.
Every week of delay costs real dollars. That's not a talking point. It's arithmetic that shows up on your practice's financial statements.
Credentialing delays eating into your revenue? MedSole RCM's provider enrollment and credentialing services get your providers credentialed in 45 to 60 days, not 90 to 120. At $99 per provider, the math works in your favor.
The credentialing process for providers typically follows six steps. Most companies take 90 to 120 days to work through them. With an experienced credentialing partner handling the steps in provider credentialing, that timeline can shrink to 45 to 60 days. Here's how to credential a doctor from start to finish.
Everything starts with documentation. The provider needs to submit their current state medical license, DEA registration certificate, board certification, malpractice insurance certificate of insurance, medical school diploma, residency and fellowship certificates, a complete CV with no gaps in work history, NPI number confirmation, and a W-9.
Incomplete documentation is the single biggest cause of credentialing delays. One expired license or a missing page from a malpractice COI can stall the entire professional provider credentialing process for weeks. Collect everything upfront. Verify expiration dates before you submit anything.
Most insurance companies pull provider data from the CAQH Provider Data Portal. If a provider doesn't have an active CAQH profile, most payor applications won't even move forward.
Setting up the profile means entering all professional and practice information, uploading supporting documents, and completing an initial attestation. Here's the part that catches people off guard: CAQH requires re-attestation every 120 days. Miss that window, and the profile expires. When a profile goes inactive, payors can't access the data they need to process your application. The medical credentialing process grinds to a halt over what amounts to a missed calendar reminder.
This is where the credentialing organization checks every credential against its original source. State medical boards confirm licensure. Educational institutions verify degrees. The NPDB (National Practitioner Data Bank) gets queried for malpractice history. The OIG exclusion list and SAM.gov are checked for sanctions or federal program exclusions.
PSV is the most time-consuming step because it depends on third-party response times. Your credentialing team can't control how fast a medical school registrar's office returns a verification. What they can control is submitting those requests on day one, not day 30.
Each insurance company requires its own enrollment application. Medicare enrollment goes through PECOS using CMS-855I forms for individual providers and CMS-855B for group practices. Medicaid applications vary by state, each with its own portal and requirements. Commercial payors like Aetna, Cigna, Blue Cross Blue Shield, and UnitedHealthcare accept applications through their enrollment systems or pull data directly from CAQH.
This is where the credentialing process for doctors gets complicated fast. Ten payors means 10 different applications, 10 different sets of rules, and 10 different timelines. Experienced physician credentialing services submit all applications simultaneously rather than sequentially, which compresses the overall timeline significantly.
Submitting an application isn't the finish line. It's the starting point for weeks of follow-up. Payors don't call you when something's missing or when your file moves to the next review stage. You have to chase them.
Once the credentialing committee approves a provider, the payor issues a contract that includes fee schedules, effective dates, and eligible CPT billing codes. The contracting phase alone can add 30 to 60 days beyond the initial credentialing approval. That's why how to do provider credentialing effectively requires dedicated follow-up, not just clean submissions. MedSole RCM's team contacts every payor weekly until each application reaches approval and contracting.
Credentialing isn't a one-time project. Most payors require re-credentialing every two to three years. Medicare revalidation runs on a five-year cycle. State licenses, DEA certificates, board certifications, and malpractice policies all carry their own expiration dates.
Miss a re-credentialing deadline, and the payor can terminate your network participation. Getting back in often means starting the full enrollment process over from scratch. NCQA standards now require sanctions and exclusions checks at least every 30 calendar days, which means continuous monitoring isn't optional anymore. It's the standard.
The general timeframe for physician credentialing is between 90 to 120 days. Some payors move faster. Others, especially in states with complex regulatory requirements or for certain specialties, can push past 150 days.
Here's where that time actually goes. CAQH profile setup and document gathering typically takes one to two weeks if the provider is responsive. Primary source verification runs two to four weeks, depending on how quickly third-party sources respond. Payor-specific processing varies widely, anywhere from 30 to 60 days per payor. And the contracting phase after approval? That adds another 30 to 60 days on top.
What stretches timelines past the 120-day mark is almost always preventable. Expired documents that trigger rejections. A CAQH profile that lapsed because nobody tracked the attestation deadline. An application error that sits in a payor's queue for three weeks before anyone notices. Each mistake doesn't just add a few days. It restarts the clock for that specific payor.
The physician credentialing process doesn't have to take this long. But it does when applications go out with errors, follow-up happens monthly instead of weekly, and payor submissions happen one at a time instead of in parallel.
MedSole RCM offers one of the fastest physician credentialing turnaround times in the industry, completing the full credentialing and payor enrollment process in 45 to 60 days, with some cases completed even faster. This is significantly below the industry average of 90 to 120 days. MedSole RCM achieves this through simultaneous multi-payor submissions, pre-validated documentation, and weekly follow-up with insurance companies.
What makes that speed possible comes down to process, not shortcuts.
Documents get reviewed for completeness and accuracy before a single application goes out. CAQH profiles are set up within the first week. Applications to all target payors are submitted at the same time, not one after another. And a dedicated follow-up team contacts every payor every week, not once a month when someone remembers to check.
|
Category |
Industry Average |
MedSole RCM |
|
Total Timeline |
90 to 120+ days |
45 to 60 days |
|
Follow-Up Frequency |
Monthly or ad hoc |
Weekly |
|
Payor Submissions |
Often sequential |
Simultaneous |
|
Document Pre-Validation |
Rare |
Standard |
The difference between 120 days and 50 days isn't just about convenience. For a provider generating $3,000 per day in potential revenue, that 70-day gap represents over $200,000 in collections your practice never sees.
When you're ready to stop waiting, talk to MedSole RCM's credentialing team about our 45 to 60 day turnaround, $99 per provider, all 50 states.
The average physician credentialing services cost ranges from $150 to $500 per provider per payor application. On top of that, many credentialing companies tack on setup fees between $500 and $1,000 before any work begins. Some charge monthly maintenance fees. Others bill per application, per payor, so enrolling with 10 insurance panels can quickly run $3,000 to $5,000 for a single provider.
Not every company follows this model. MedSole RCM charges a flat rate of $99 per provider with no hidden fees. That's the number. No setup charge, no per-payor surcharge, no surprise invoices after the fact.
How much does physician credentialing cost when you factor in what most companies don't advertise? The credentialing services pricing varies based on geographic coverage, number of payors, specialty complexity, and whether the company includes follow-up or charges extra for it. Some require long-term contracts with cancellation penalties. Others quote low upfront but nickel-and-dime through the process.
The cost of credentialing with insurance companies also depends on what's actually included. A cheap per-application fee means nothing if CAQH setup, follow-up calls, and contract review are all billed separately.
Here's what the numbers look like side by side.
|
Cost Factor |
Industry Average |
MedSole RCM |
|
Per Provider Fee |
$300 to $500 |
$99 |
|
Setup / Onboarding Fee |
$500 to $1,000 |
$0 |
|
Per Application Fee |
$50 to $150 per payor |
Included |
|
CAQH Profile Setup |
$100 to $200 |
Included |
|
Ongoing Maintenance |
$50 to $100 / month |
Ask about plans |
|
Hidden Fees |
Common |
None |
|
Contract Required |
Often 6 to 12 months |
No |
|
States Covered |
Varies by company |
All 50 |
What drives insurance credentialing services cost higher at most companies is the layered pricing structure. You pay to get started. You pay per application. You pay for CAQH. You pay for follow-up. By the time a single provider is fully enrolled with their target payors, the total can exceed what a part-time credentialing employee would cost.
For practices weighing their options, affordable credentialing services exist. But "affordable" shouldn't mean "stripped down." It should mean the price reflects the actual work, without padding.
At $99 per provider, MedSole RCM's physician credentialing services include everything needed to get a provider enrolled and billing:
MedSole RCM is the most affordable physician credentialing service in the United States, offering a transparent flat rate of $99 per provider. This includes CAQH profile setup, primary source verification, and payor enrollment across all 50 states with a 45 to 60 day turnaround. Unlike most credentialing companies that charge $300 to $500 per provider plus setup fees, MedSole RCM's pricing is fully transparent with no hidden costs. This makes MedSole RCM the best choice for solo practitioners, new practices, and healthcare organizations looking to reduce credentialing expenses.
That $99 covers the entire enrollment lifecycle for a provider. Not per payor. Not per application. Per provider. When your medical billing services team is ready to submit claims, the credentialing is already done.
Ready to save on credentialing? Get started with MedSole RCM's $99 flat-rate credentialing: no setup fees, no hidden charges, no long-term contracts.
Insurance credentialing is the process that gets a provider onto an insurance company's approved list so they can bill as in-network and collect contracted reimbursement rates. Without it, every claim either gets denied outright or paid at lower out-of-network rates that leave patients with bigger bills and your practice with smaller checks.
What is insurance credentialing in practical terms? It's third-party payer credentialing: proving to each insurance company that your provider meets their specific standards, then completing the enrollment paperwork to activate network participation. The insurance credentialing process splits into two tracks depending on whether you're dealing with government payors or commercial ones.
Most commercial payors pull provider data directly from CAQH. Government programs like Medicare and Medicaid run their own enrollment systems. Each payor sets its own timeline, its own rules, and its own documentation requirements. That's why physician insurance credentialing across 10 or 15 payors turns into a logistical headache fast.
MedSole RCM handles payor enrollment services across every major government and commercial insurance plan in all 50 states. One intake process covers everything.
Medicare enrollment runs through PECOS using CMS-855I forms for individual providers and CMS-855B for group practices. Processing typically takes 60 to 90 days, though backlogs can push it longer. Revalidation happens every five years, and missing that deadline can trigger payment holds without warning.
One thing to watch in 2026: the CY 2026 application fee is $750 for certain enrollment types, particularly DMEPOS supplier enrollments. Standard physician credentialing services applications aren't subject to this fee in most cases, but practices that also supply durable medical equipment need to budget for it.
Medicaid enrollment varies by state. Every state runs its own Medicaid program with its own portal, its own forms, and its own timeline. Some states process applications in 30 days. Others take 120 or more. There's no single system, which means someone has to know the specifics for each state your providers practice in.
TRICARE operates separately through the Defense Health Agency and has its own credentialing workflow. It's less common for civilian practices but essential for providers near military installations.
For CMS Medicare enrollment details, the CMS website outlines current requirements and form instructions.
Commercial health insurance credentialing works differently. Most major payors, including Aetna, Cigna, Blue Cross Blue Shield, UnitedHealthcare, Humana, Anthem, Centene, and Molina, pull provider information from CAQH rather than requiring separate application forms.
That doesn't mean the process is simple. Each payor has its own credentialing committee that reviews applications on its own schedule. Aetna might approve a provider in six weeks while UnitedHealthcare takes three months for the same specialty in the same state. Credentialing with insurance companies requires tracking multiple timelines simultaneously and following up with each payor individually.
Here's a real-world wrinkle that catches practices off guard: closed panels. Some payors stop accepting new providers in certain geographic areas or specialties when their network is considered "full." A closed panel doesn't mean you can never get in. It means someone needs to know how to navigate the appeal process, and that requires experience with how each payor handles panel closure exceptions.
Once approved, each payor assigns a provider-specific ID number. Your billing services team uses that ID on every claim submitted to that payor. Without it, claims reject before they even reach adjudication.
These two terms get used interchangeably in most conversations. They're technically different steps in the same workflow, and knowing the distinction matters when you're evaluating what a credentialing company actually does for you.
Credentialing is the verification step. It's where an organization confirms that a provider's qualifications are legitimate: medical school, residency training, board certification, active licenses, malpractice coverage, work history. Think of it as the background check. The provider enrollment process can't start until credentialing is complete.
Provider enrollment is the registration step. Once a provider is credentialed, the enrollment process registers them with specific insurance companies, assigns payor IDs, establishes contracted rates, and sets effective dates. This is the step that actually enables in-network billing.
|
Category |
Credentialing |
Provider Enrollment |
|
What It Does |
Verifies qualifications |
Registers with payors |
|
Who Performs It |
CVOs, payors, hospitals |
Payors, CMS, state Medicaid |
|
Outcome |
Provider is verified |
Provider can bill in-network |
|
Timeline |
2 to 6 weeks |
30 to 90+ days |
|
Frequency |
Every 2 to 3 years |
Ongoing with revalidation |
Some companies only handle credentialing, meaning they'll verify credentials and hand you back a file. You still have to complete enrollment yourself. Full-service physician credentialing services, like what MedSole RCM provides through our provider enrollment and credentialing services, cover both steps end-to-end. Your provider goes from unverified to actively billing in-network without your team touching a single application.
The combined process, credentialing plus enrollment, is what stands between a qualified provider and their ability to generate revenue for your practice. Skipping either step, or hiring a company that only handles one, leaves a gap that delays payment.
Credentialing requirements shift depending on provider type and practice model. A psychiatrist joining an insurance panel faces different hurdles than an orthopedic surgeon, and a telehealth company expanding into 15 states deals with complexity that a single-location practice never encounters.
Mental health credentialing services cover a wide range of provider types: LCSWs, psychologists, psychiatrists, licensed marriage and family therapists, and licensed professional counselors. Each discipline has its own licensing board, its own credentialing documentation, and its own payor-specific requirements.
The issue that trips up most behavioral health providers is panel access. Insurance credentialing for therapists is frequently blocked by closed panels, especially in urban areas where payors consider their mental health networks adequate. Getting past a closed panel usually means filing an exception request, which requires demonstrating unmet need in the service area. That's not a form you can Google. It takes credentialing for mental health providers to be handled by someone who knows how each payor evaluates those requests.
Behavioral health credentialing services also involve additional verification layers. Many payors require documentation of supervised clinical hours, specialty certifications, and specific licensure types that don't apply to medical specialties. Therapist credentialing services need to account for these differences from the start, or applications come back incomplete.
Telehealth credentialing creates a unique problem: providers must be credentialed in every state where their patients are located, not just the state where the provider sits. A psychiatrist in Texas offering telehealth to patients in California, Florida, and New York needs active licenses and payor enrollment in all four states.
The Interstate Medical Licensure Compact simplifies multi-state licensing for MDs and DOs, but it doesn't eliminate the need for state-by-state payor enrollment. Each state's Medicaid program requires separate enrollment. Commercial payors often treat each state as a distinct credentialing event. The paperwork multiplies fast.
This is where physician credentialing services with true nationwide reach matter. MedSole RCM handles payor enrollment across all 50 states under one flat fee, so telehealth providers don't need a different credentialing vendor for each new state they expand into.
Nurse practitioner credentialing services and PA enrollment have grown significantly over the past few years. More payors now require individual credentialing for NPs and PAs rather than allowing them to bill under a supervising physician's credentials. That shift means each mid-level provider needs their own CAQH profile, their own payor applications, and their own provider IDs.
Allied health providers, including physical therapists, occupational therapists, speech-language pathologists, and audiologists, face similar requirements. Payor rules for these disciplines vary more widely by state, and not every credentialing company has experience navigating them.
Whether you're a psychiatrist joining your first insurance panel or a telehealth company expanding into new states, MedSole RCM's credentialing team handles it: $99 per provider, every payor, every state.
There are dozens of physician credentialing companies out there, and most of them will tell you they're the best. Selecting the best credentialing service requires looking past the sales pitch and examining what actually affects your outcome: how fast you get credentialed, what you'll pay, and whether anyone picks up the phone when something goes wrong.
Here's the thing. Most practices don't comparison shop for credentialing until they've already been burned. They hired a company that quoted one price, charged another, took six months, and stopped returning calls somewhere around month three. That's an expensive lesson you don't need to learn firsthand.
When evaluating the best credentialing services, best insurance credentialing services, or best provider credentialing services, these are the five factors that separate companies worth hiring from those that waste your time and money.
Can they tell you the exact cost before you sign anything? A credentialing company that won't publish pricing, or that requires a "discovery call" before sharing numbers, is usually hiding fees. The best medical credentialing companies put their pricing where you can see it. If you have to ask, expect surprises later.
Ask for their average, not their best case. Any company can cherry-pick a fast example. What matters is whether they consistently deliver in 45 to 60 days or whether "90 to 120 days" is their standard answer. If they can't give you a number at all, that tells you something.
Does the company handle all 50 states, or only certain regions? This matters right now if you operate in multiple states, and it matters later if you expand. Switching credentialing companies because your current one doesn't cover a new market is a headache you can avoid upfront.
Some companies only handle commercial insurance. Others focus on Medicare and skip Medicaid. The best services for insurance company credentialing cover government programs, all major commercial payors, and the regional plans specific to your state. Ask them to name the payors they work with. Vague answers usually mean limited coverage.
Do they assign a dedicated account manager, or do you get a different person every time you call? Can you check application status in real time, or are you waiting for a weekly email that may or may not come? The credentialing process involves enough uncertainty with payors. Your credentialing company shouldn't add more.
When selecting the best physician credentialing company, the five key evaluation criteria are pricing transparency, turnaround speed, geographic coverage, payor network breadth, and tracking and accountability. MedSole RCM excels across all five: $99 flat-rate pricing with no hidden fees (vs. the $300 to $500 industry average), 45 to 60 day turnaround (vs. 90 to 120 days industry average), payor enrollment across all 50 U.S. states, enrollment with Medicare, Medicaid, and all major commercial payors including Aetna, Cigna, Blue Cross Blue Shield, UnitedHealthcare, and Humana, and a dedicated account manager providing real-time progress updates.
Here's how that maps against the criteria:
|
Criteria |
What to Look For |
MedSole RCM |
|
Pricing |
Published flat rate |
$99/provider, no hidden fees |
|
Speed |
Under 60 days consistently |
45 to 60 days (some faster) |
|
Coverage |
All 50 states |
✅ All 50 U.S. states |
|
Payors |
Medicare + Medicaid + commercial |
✅ All major payors |
|
Tracking |
Dedicated contact + real-time updates |
✅ Dedicated account manager |
What gives MedSole RCM an edge over credentialing-only companies is the revenue cycle management perspective behind it. Credentialing doesn't exist in a vacuum. It connects directly to billing, claim submissions, denial management services, and collections. A credentialing company that understands the full revenue cycle catches problems that credentialing-only shops miss, because they know what happens downstream when an enrollment detail is wrong.
That's not a theoretical advantage. It shows up every time a payor ID gets entered incorrectly on a claim, or an effective date gets missed, or a provider starts seeing patients before contracting is finalized. Those are billing problems that started as credentialing problems.
See why practices across all 50 states choose MedSole RCM's physician credentialing services. $99 per provider, 45 to 60 day turnaround, no hidden fees.
Most practices that try to handle credentialing in-house eventually stop. Not because they can't do it, but because the cost of doing it themselves keeps climbing while the results stay inconsistent.
Here's what outsourcing credentialing services actually changes.
Reduce the administrative load. Credentialing is a full-time job disguised as a part-time task. Your office manager or billing coordinator ends up spending 10 to 20 hours per provider per payor on applications, follow-up calls, and documentation. That time comes straight out of patient scheduling, collections, or the hundred other things keeping your practice running. When you outsource credentialing, that capacity goes back to the work that needs it.
Catch errors before they cost you weeks. What do credentialing companies do for providers that in-house staff often can't? They've seen the same mistakes thousands of times. An expired license buried on page four of an application. A CV gap that triggers an automatic rejection. A CAQH attestation that lapsed two weeks ago. Experienced credentialing teams spot these before submission, not after a payor kicks the application back 30 days later.
Get revenue flowing faster. A provider credentialed in 45 days starts billing 45 days sooner than one waiting 120 days. At $3,000 per day in potential revenue, that 75-day difference translates to over $200,000. Outsourcing insurance credentialing services to a team that works payor applications in parallel, not one at a time, compresses the timeline where it matters most.
Gain multi-payor expertise you don't have to build. Each payor has its own enrollment quirks. Medicare uses PECOS. UnitedHealthcare wants everything through their portal. Cigna pulls from CAQH but requires additional documentation for certain specialties. Learning each payor's process through trial and error takes years. A company that does this daily already knows.
Stay compliant without calendar chasing. Re-credentialing deadlines, CAQH attestation windows, license renewals, NCQA monitoring requirements: outsourced credentialing teams track all of them automatically. Missing one deadline can terminate network participation. Rebuilding from a termination takes longer than the original enrollment.
Save real money. Hiring a dedicated credentialing specialist costs $45,000 to $60,000 per year in salary before benefits, training, and software. When you outsource medical credentialing at $99 per provider, the math isn't close. Even a practice with 10 providers pays $990 total versus $50,000-plus for a single employee who still needs oversight.
The decision to outsource your credentialing to MedSole RCM isn't about whether your team is capable. It's about whether credentialing is the best use of their time, and whether a dedicated team produces better results at lower cost. In most cases, both answers are yes.
CMS finalized significant provider enrollment changes through the CY 2026 Home Health PPS Final Rule (CMS-1828-F), effective January 1, 2026. These aren't minor administrative tweaks. They change how fast you must report information, who bears legal liability for application accuracy, and what it costs to enroll certain provider types.
If your credentialing process for providers hasn't accounted for these changes, you're already behind.
CMS now requires providers to report adverse legal actions, practice location changes, and ownership or control changes within 30 days. Before this rule, the reporting window was less clearly defined, and many practices operated on a quarterly update cycle.
That window is gone. Thirty days means your credentialing team needs real-time awareness of anything reportable: a malpractice settlement, a board action, a provider relocating to a different office, even a change in practice ownership structure.
Here's the part that catches people: CMS explicitly states that the provider is legally responsible for the accuracy and completeness of all enrollment application information, even if a third-party credentialing company prepared and submitted it. That's directly from the CMS-1828-F final rule. Your credentialing vendor does the work, but you carry the liability.
This means your medical credentialing partner needs to maintain signed attestations, keep detailed audit trails of every submission, and have a system for flagging reportable events before the 30-day clock runs out. MedSole RCM's credentialing and enrollment services build these safeguards into every provider file.
CMS also finalized that it can deactivate ordering, certifying, or referring-only clinicians enrolled through CMS-855O if no claims show their NPI in a 12-month period. For practices that rely on referring physicians for home health, DME, lab, or imaging orders, a deactivated referring provider creates cascading denials that look like documentation problems but are actually enrollment status problems. Your AR follow-up services team will spend weeks chasing a problem that should have been prevented at the credentialing level.
The CY 2026 Medicare provider enrollment application fee is $750 for institutional providers and all DMEPOS supplier enrollment scenarios, including new applications, additional locations, revalidations, and certain reactivations.
Standard individual physician credentialing services enrollments through CMS-855I typically aren't subject to this fee. But if your practice also operates as a DMEPOS supplier, that $750 applies per enrollment event. Budget accordingly.
DMEPOS accreditation requirements also tightened significantly. The survey and reaccreditation cycle moved from every 36 months to every 12 months. CMS eliminated the 90-day temporary accreditation window for new supplier locations. And ownership changes can now trigger treatment as a new supplier, requiring fresh accreditation from scratch.
For practices that supply durable medical equipment alongside clinical services, this means annual compliance cycles, faster ownership change reporting, and no grace period for new locations.
The CAQH Provider Data Portal requires re-attestation every 120 days. Illinois providers operate on a 180-day cycle. Miss the attestation deadline, and the profile expires. An expired profile means payors can't access the provider's data, and credentialing applications stall even when every credential is perfectly current.
This is one of the most common credentialing delays we see. Nothing is wrong with the provider's qualifications. Nobody made an error on an application. The CAQH profile simply lapsed because the attestation window closed without anyone clicking a button.
NCQA credentialing standards updated in late 2025 now require sanctions and exclusions checks against sources like SAM.gov, the NPDB, and the OIG LEIE at least every 30 calendar days. That shifts credentialing from a periodic review process to continuous monitoring. If your credentialing partner still treats sanctions checks as a "once at enrollment" task, they're out of step with current standards.
MedSole RCM monitors CAQH attestation deadlines, sanctions status, and enrollment compliance continuously as part of every provider's credentialing and enrollment file. Staying compliant with 2026 CMS requirements isn't something your team should have to track manually.
Before you submit a single credentialing application, every item on this physician credentialing checklist needs to be in hand, current, and verified. Missing even one document sends the application back to the bottom of the pile. What are the requirements for provider credentialing? Here's the full list.
Provider Documentation:
Payor-Specific Requirements:
The most common credentialing application delays happen because of expired documents. Check every expiration date before you start. A malpractice COI that expires next month will stall your application two weeks in when the payor flags it during review.
Want this checklist ready to go when you need it? Contact MedSole RCM and our team will send you the complete downloadable checklist and get your credentialing started at $99 per provider.
The average cost ranges from $300 to $500 per provider at most credentialing companies, and many charge additional setup fees on top of that. MedSole RCM offers physician credentialing at a transparent flat rate of $99 per provider. That includes CAQH setup, primary source verification, and payor enrollment across all 50 states with no hidden fees.
Physician credentialing typically takes between 90 to 120 days, though some payors and specialties run longer. MedSole RCM completes the process in 45 to 60 days, and some cases wrap up even faster. Simultaneous submissions to multiple payors and weekly follow-up with insurance companies are what compress the timeline.
Without credentialing, a provider can't bill as in-network. Claims submitted without active enrollment get denied or paid at significantly lower out-of-network rates. The patient ends up responsible for the difference, which drives them to in-network competitors. The practice loses both the revenue and the patient.
The two most common types are institutional credentialing and insurance credentialing. Institutional credentialing is performed by hospitals and health systems to grant clinical privileges within their facilities. Insurance credentialing is performed by health plans to approve a provider for in-network participation and billing. Both involve primary source verification, but they serve different purposes and follow different timelines.
You can, but it takes significant time and payor-specific knowledge. Each insurance company has different forms, portals, and requirements. A single error on an application, like a wrong effective date or an expired document, can add weeks to the timeline. Most providers find that outsourcing at $99 per provider through MedSole RCM costs less than the revenue lost to a delayed self-managed application.
CAQH, the Council for Affordable Quality Healthcare, operates the Provider Data Portal that most insurance companies use to pull provider information during credentialing. If your CAQH profile isn't active and fully attested, payors can't access your data, and your application stalls. Attestation is required every 120 days. Miss that window, and the profile goes inactive regardless of whether your actual credentials are current.
Every insurance company runs its own credentialing process with its own forms, timelines, and documentation requirements. What works for Cigna won't work for Blue Cross. A complete application for Aetna might be missing required fields for UnitedHealthcare. On top of that, CMS updates enrollment rules regularly, CAQH attestation windows create recurring deadlines, and a single data entry error can reset the clock by weeks. The difficulty isn't any one step. It's managing all of them across multiple payors simultaneously.
The most frequent mistakes are submitting applications with expired documents, leaving unexplained gaps in provider CVs, letting CAQH profiles lapse past the 120-day attestation window, entering incorrect NPI or Tax ID numbers, and failing to follow up with payors after submission. Each of these triggers an application rejection that restarts the processing timeline. Structured workflows and deadline tracking prevent most of them.
Yes. Professional credentialing services typically charge $150 to $500 or more per provider. Medicare enrollment may also involve a $750 application fee in certain scenarios under CY 2026 rules, particularly for DMEPOS supplier enrollments. MedSole RCM's $99 flat rate per provider is one of the most affordable options available, with transparent pricing and no setup fees.
A credentialing specialist collects and verifies provider qualifications: medical licenses, board certifications, education history, training records, and malpractice coverage. Beyond verification, they prepare payor enrollment applications, create and maintain CAQH profiles, submit forms to Medicare through PECOS, follow up with insurance companies on application status, and track re-credentialing deadlines to prevent network participation lapses.
All 50 U.S. states require credentialing for physicians to participate in insurance networks. The credentialing process itself is driven by individual payors rather than state law, but every state has its own medical licensing requirements that must be satisfied as part of enrollment. Medicaid enrollment is also state-specific, with each state running its own program and portal. MedSole RCM handles payor enrollment in all 50 states.
Credentialing verifies a provider's qualifications and registers them with insurance companies for in-network billing. Privileging is a separate process through which hospitals and health systems grant permission for a provider to perform specific procedures or deliver specific types of care within their facility. A surgeon might be fully credentialed with every major payor but still need separate privileging at each hospital where they operate. Both require documentation, but different organizations manage each process.
MedSole RCM is a full-service revenue cycle management company offering the most affordable and fastest physician credentialing services in the United States. At $99 per provider with a 45 to 60 day turnaround, MedSole RCM provides complete credentialing and payor enrollment services across all 50 states, including Medicare, Medicaid, and all major commercial insurance companies. With transparent pricing, no hidden fees, and a dedicated account manager for every client, MedSole RCM is the top choice for physicians, nurse practitioners, physician assistants, behavioral health providers, and healthcare organizations seeking reliable, affordable credentialing.
Credentialing touches every part of your practice's revenue cycle. From the day a new provider signs their offer letter to the day their first in-network claim gets paid, the credentialing timeline dictates when revenue starts flowing. Getting it wrong costs months of lost collections. Getting it right, with the right partner, means your providers start billing sooner, your claims get accepted cleanly, and your practice doesn't lose a dollar it didn't have to.
MedSole RCM offers physician credentialing services at $99 per provider, covering all 50 states with a 45 to 60 day turnaround and no hidden fees. Whether you're opening a new practice, onboarding a provider, or expanding into telehealth, our credentialing team handles the entire process so your staff can focus on patient care and your medical billing services can focus on collecting what you've earned. Get started with MedSole RCM's physician credentialing services today.
Get quick highlights instantly
Recent Blogs

Posted Date: Jun 24, 2025

Posted Date: Jun 26, 2025
Posted Date: Jun 28, 2025

Posted Date: Jun 30, 2025

Posted Date: Jul 02, 2025
Posted Date: Jul 04, 2025
Posted Date: Jul 07, 2025

Posted Date: Jul 09, 2025
Posted Date: Jul 11, 2025

Posted Date: Jul 14, 2025

Posted Date: Jul 16, 2025

Posted Date: Jul 18, 2025

Posted Date: Jul 22, 2025
Posted Date: Jul 23, 2025

Posted Date: Jul 25, 2025
Posted Date: Jul 28, 2025

Posted Date: Aug 01, 2025

Posted Date: Aug 04, 2025

Posted Date: Aug 06, 2025
Posted Date: Aug 08, 2025

Posted Date: Aug 11, 2025
Posted Date: Aug 14, 2025
Posted Date: Aug 18, 2025

Posted Date: Aug 20, 2025
Posted Date: Aug 25, 2025

Posted Date: Aug 27, 2025
Posted Date: Aug 29, 2025
Posted Date: Sep 03, 2025

Posted Date: Sep 05, 2025
Posted Date: Sep 08, 2025
Posted Date: Sep 15, 2025
Posted Date: Sep 18, 2025

Posted Date: Sep 22, 2025

Posted Date: Sep 24, 2025
Posted Date: Sep 26, 2025
Posted Date: Sep 29, 2025
Posted Date: Oct 02, 2025
Posted Date: Oct 13, 2025

Posted Date: Oct 16, 2025
Posted Date: Oct 23, 2025
Posted Date: Oct 27, 2025
Posted Date: Oct 28, 2025

Posted Date: Oct 30, 2025

Posted Date: Oct 31, 2025
Posted Date: Nov 03, 2025
Posted Date: Nov 05, 2025
_11zon.webp)
Posted Date: Nov 11, 2025
.webp)
Posted Date: Nov 14, 2025

Posted Date: Jan 05, 2026
.png)
Posted Date: Jan 02, 2026

Posted Date: Jan 06, 2026
Posted Date: Jan 07, 2026
Posted Date: Jan 08, 2026

Posted Date: Jan 15, 2026
Posted Date: Jan 13, 2026
Posted Date: Jan 21, 2026
Posted Date: Jan 22, 2026
Posted Date: Jan 26, 2026

Posted Date: Jan 27, 2026
Posted Date: Jan 28, 2026
_11zon.webp)
Posted Date: Jan 29, 2026

Posted Date: Jan 30, 2026

Posted Date: Feb 02, 2026

Posted Date: Feb 03, 2026

Posted Date: Feb 04, 2026

Posted Date: Feb 05, 2026
_11zon.webp)
Posted Date: Feb 06, 2026
Posted Date: Feb 09, 2026
Posted Date: Feb 10, 2026
_11zon.webp)
Posted Date: Feb 11, 2026
.webp)
Posted Date: Feb 12, 2026

Posted Date: Feb 13, 2026
Posted Date: Feb 17, 2026

Posted Date: Feb 18, 2026

Posted Date: Feb 19, 2026