Posted By: Medsole RCM
Posted Date: Oct 02, 2025
Introduction
In healthcare industry the behavioral health practices are expanding as awareness of mental health is growing day by day and managing the financial side of these services requires specialized billing knowledge. Many healthcare providers face a lot of challenges, including complex coding, insurance-specific guidelines, and changing regulations. For healthcare practices that are providing services of counseling, psychiatry, or therapy, accurate claim submission is important for financial growth.
MedSole RCM understands the unique needs of behavioral health professionals. Our services are designed to help practices overcome the common hurdles that often result in claim denials or delayed payments. This blog explores the details of billing for mental health services, covering billing codes, payer rules, and solutions that improve revenue cycle efficiency.
Billing for behavioral health services mostly involves a wide range of CPT and ICD-10 codes. These codes are different from general medical billing and depends on session length, type of therapy, and the credentials of healthcare provider. There will be the rejected claims if even small detail is missing, such as the duration of therapy or whether it was an individual or group session.
There is a requirement of prior authorization by many insurance plans before covering counseling, psychiatric evaluations, or therapy sessions. In case of missing or expired authorization, claims are mostly denied. This may add extra administrative work for healthcare providers who are already managing the patient care.
Unlike general healthcare billing, reimbursement policies for psychiatry billing services or therapy billing services are not consistent across payers. Some carriers cover teletherapy, while others do not. Some reimburse only for licensed psychologists but not for counselors. Understanding these differences is essential for reducing payment delays.
Behavioral health billing services take care of claims, their submission, and follow-up. These services help healthcare practices to reduce administrative burdens, avoid errors, and assist in faster reimbursements. With expert behavioral health billing company like MedSole RCM, healthcare providers can focus more on patient care and the claims are handled correctly.
Behavioral health billing codes cover a lot of services, from initial psychiatric assessments to regular therapy sessions. Correct use of codes is very important for successful reimbursement.
Billing for behavioral health services requires proper detail and attention. Healthcare providers should consider session duration, service type, and provider qualifications while submitting the claims. There will be the claim rejections if data in incorrect or missing.
Professional behavioral health billing services can manage these steps effectively, avoiding common mistakes that slow down payments.
When selecting a behavioral health billing company, providers should look for a team with experience in mental health claims. MedSole RCM specializes in handling the unique demands of psychiatry billing services and therapy billing services.
Psychiatrists mostly face complex reimbursement challenges due to the variety of services they are providing, from diagnostic evaluations to medication management. Psychiatry billing services offers that claims should show the detail and type of care delivered.
These services are very important for psychiatrists working with both therapy and medication management. Without accurate billing support, providers will be having a risk of payment or denials.
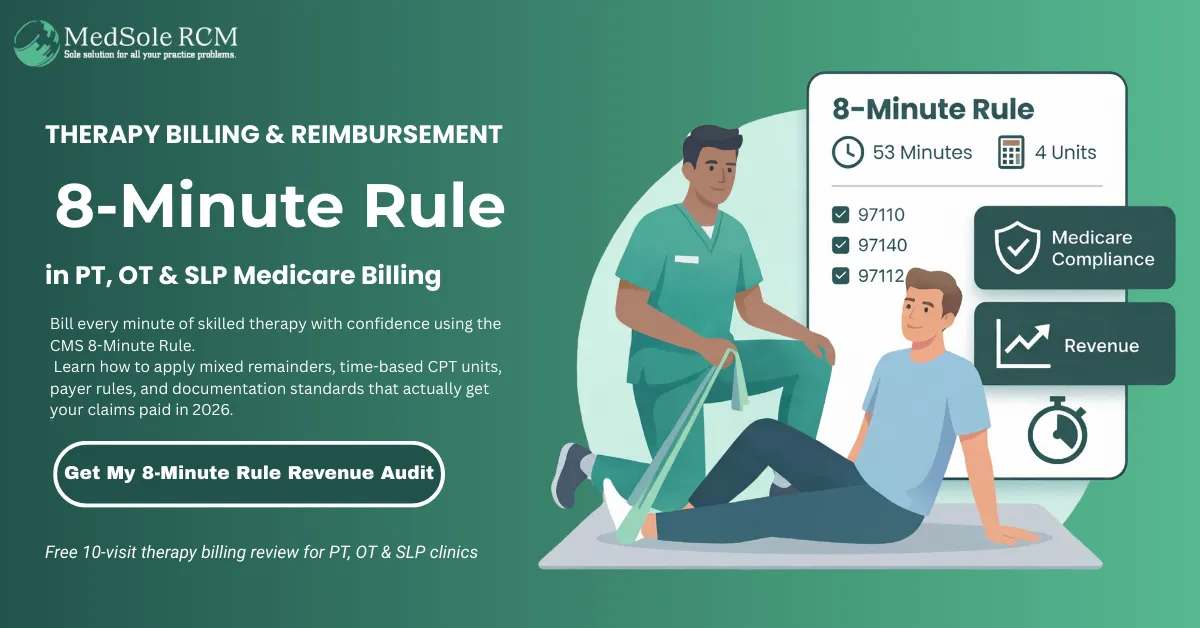
Therapy billing services focus on accurate claim submission for individual, group, and family therapy sessions. The time-based nature of therapy codes requires careful documentation. For example, a 30-minute session and a 60-minute session fall under different CPT codes.
Billing for therapists mostly becomes complicated when insurance coverage allows limited sessions per year. Professional billing services help to manage these limitations by tracking authorizations and checking that claims should be correctly submitted.
Billing for therapists requires proper attention and detail as many practices consist of solo practitioners or small groups. These providers usually don’t have the staff to manage complex claim processes. Outsourcing billing helps therapists to maintain their focus on patients instead of paperwork.
MedSole RCM supports billing for therapists by providing exceptional services of claim preparation, submission, follow-up, and denial management. In the result of this, small practices remain financially stable while delivering quality care.
Billing in the behavioral health field is mostly more challenging than in other areas of healthcare due to complex coding, insurance-specific rules, and regular authorization requirements. MedSole RCM provides professional support and healthcare practices gain access to proper knowledge in behavioral health billing services, psychiatry billing services, therapy billing services, and billing for therapists. By partnering with a trusted behavioral health billing company like MedSole RCM, healthcare providers can reduce denials, improve cash flow, and spend more time focusing on patient care. Contact our Experts and let them handle your administrative burden.
Q. Why behavioral health billing different from general medical billing?
Behavioral health billing is very different because it requires time-based coding, insurance-specific guidelines, and mental health diagnosis codes. General medical billing normally involves the procedures and lab tests, while behavioral billing is mostly focused on therapy, counseling, and psychiatric care.
Q. Why prior authorization is important in behavioral health billing services?
Many healthcare insurances require prior authorization for psychiatric evaluations or therapy sessions. Without this approval, claims mostly get denied. Behavioral health billing services handle authorization requests and track the renewals, checking that care is covered.
Q. How behavioral health billing codes affect reimbursement?
Behavioral health billing codes explains and define the type and length of service. Using incorrect codes may results is claim rejections or less reimbursement. Accurate coding results in that providers are paid for the full value of their services.
Q. Why small practices get benefit from billing for therapists services?
Small practices often lack billing staff. Billing for therapists services from MedSole RCM results in efficient claims processing, authorizations are tracked, and payments collect on time. This allows therapists to focus on patient care rather than billing and administrative work.
Q. How outsourcing improve billing for behavioral health services?
Outsourcing billing for behavioral health services provides access to specialized knowledge, reduces claim denials, and accelerate the payment. It also reduces the burden of administrative work for healthcare providers.
Q. Why should providers choose MedSole RCM as their behavioral health billing company?
MedSole RCM offers specialized expertise in psychiatry billing services, therapy billing services, and billing for therapists. Our team ensures accurate claim submission, denial management, and financial reporting, making us a reliable partner for mental health providers.
Get quick highlights instantly
Recent Blogs

Posted Date: Jun 24, 2025

Posted Date: Jun 26, 2025
Posted Date: Jun 28, 2025

Posted Date: Jun 30, 2025

Posted Date: Jul 02, 2025
Posted Date: Jul 04, 2025
Posted Date: Jul 07, 2025

Posted Date: Jul 09, 2025
Posted Date: Jul 11, 2025

Posted Date: Jul 14, 2025

Posted Date: Jul 16, 2025

Posted Date: Jul 18, 2025

Posted Date: Jul 22, 2025
Posted Date: Jul 23, 2025

Posted Date: Jul 25, 2025
Posted Date: Jul 28, 2025

Posted Date: Aug 01, 2025

Posted Date: Aug 04, 2025

Posted Date: Aug 06, 2025
Posted Date: Aug 08, 2025

Posted Date: Aug 11, 2025
Posted Date: Aug 14, 2025
Posted Date: Aug 18, 2025

Posted Date: Aug 20, 2025
Posted Date: Aug 25, 2025

Posted Date: Aug 27, 2025
Posted Date: Aug 29, 2025
Posted Date: Sep 03, 2025

Posted Date: Sep 05, 2025
Posted Date: Sep 08, 2025
Posted Date: Sep 15, 2025
Posted Date: Sep 18, 2025

Posted Date: Sep 22, 2025

Posted Date: Sep 24, 2025
Posted Date: Sep 26, 2025
Posted Date: Sep 29, 2025
Posted Date: Oct 02, 2025
Posted Date: Oct 13, 2025

Posted Date: Oct 16, 2025
Posted Date: Oct 23, 2025
Posted Date: Oct 27, 2025
Posted Date: Oct 28, 2025

Posted Date: Oct 30, 2025

Posted Date: Oct 31, 2025
Posted Date: Nov 03, 2025
Posted Date: Nov 05, 2025
_11zon.webp)
Posted Date: Nov 11, 2025
Posted Date: Nov 14, 2025

Posted Date: Jan 05, 2026
.png)
Posted Date: Jan 02, 2026

Posted Date: Jan 06, 2026
Posted Date: Jan 07, 2026
Posted Date: Jan 08, 2026

Posted Date: Jan 15, 2026
Posted Date: Jan 13, 2026
Posted Date: Jan 21, 2026
Posted Date: Jan 22, 2026
Posted Date: Jan 26, 2026

Posted Date: Jan 27, 2026
Posted Date: Jan 28, 2026
_11zon.webp)
Posted Date: Jan 29, 2026

Posted Date: Jan 30, 2026

Posted Date: Feb 02, 2026

Posted Date: Feb 03, 2026

Posted Date: Feb 04, 2026

Posted Date: Feb 05, 2026
_11zon.webp)
Posted Date: Feb 06, 2026
Posted Date: Feb 09, 2026
Posted Date: Feb 10, 2026
_11zon.webp)
Posted Date: Feb 11, 2026
.webp)
Posted Date: Feb 12, 2026

Posted Date: Feb 13, 2026
Posted Date: Feb 17, 2026

Posted Date: Feb 18, 2026

Posted Date: Feb 19, 2026
Posted Date: Feb 20, 2026
Posted Date: Feb 23, 2026
Posted Date: Feb 25, 2026

Posted Date: Feb 26, 2026