Verify Benefits and Eligibility for your Patients in the fastest way possible.

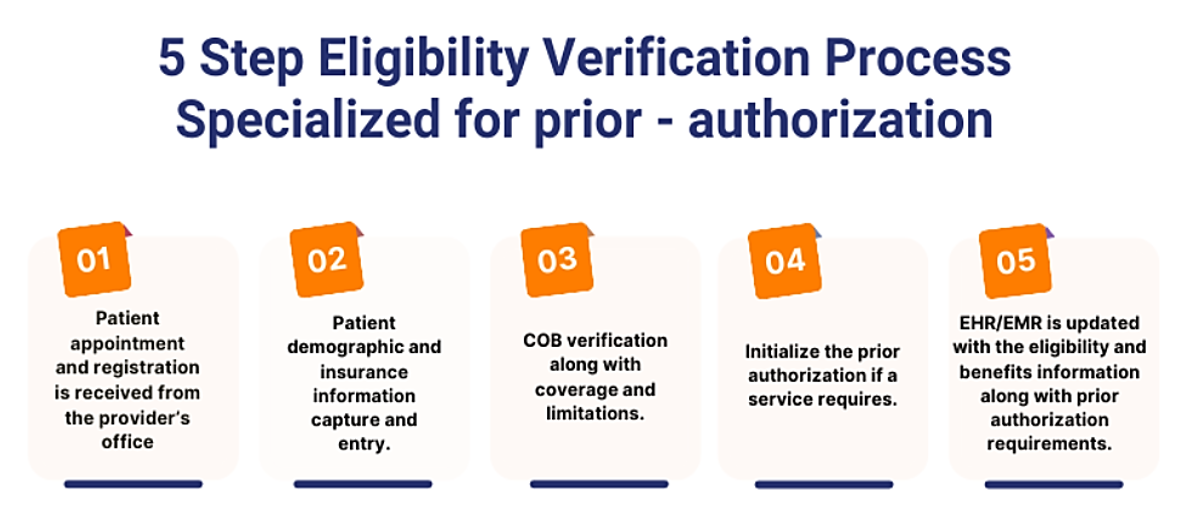
Prior authorisation is a method that allows practises to submit and recuperate approved claims in order to optimise cash flow. Poor prior authorisation processes can result in the polar opposite of what you want: more denials and less income. Healthcare providers must verify each patient’s eligibility and benefits prior to the patient’s visit in order to receive payment for services delivered. According to some estimates, up to 65% of claims are refused because the patient is ineligible for the services provided by the healthcare provider. Regrettably, it is one of the most underutilised processes in the revenue cycle chain.

- Prior authorization determination and requirements.
- Submission of authorization paperwork to insurance.
- Follow-up on the authorization request.
- Notification and resolution of rejection of authorization application.
MedSole RCMs Eligibility verification and prior authorization services offer:
- Save operational costs Improve speed to care delivery
- Reduce Claim Denials
- Reduce Bad Debits and increase Cash Collections
- Focus on growing your Business
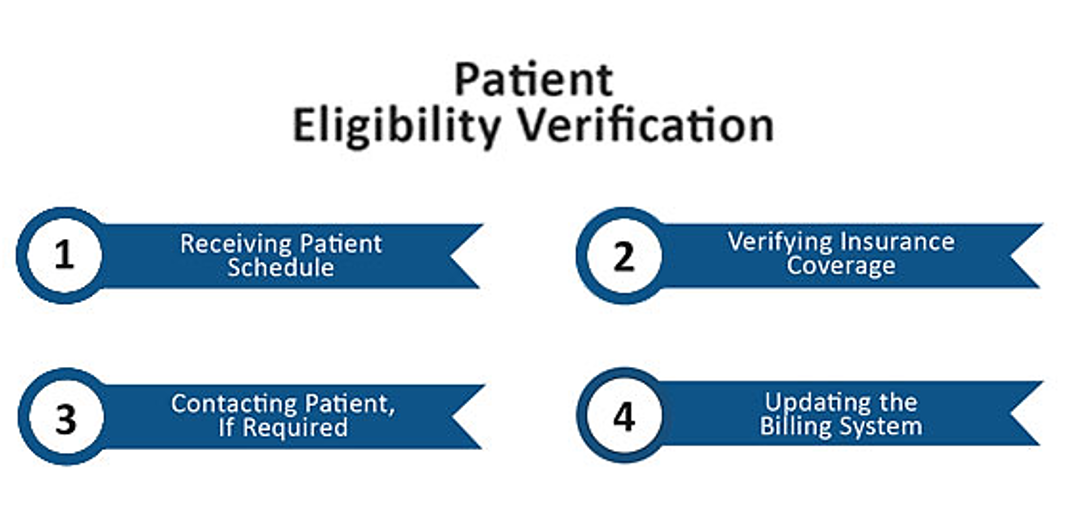
We at MedSole RCM offer our providers the most effective automated workflow to bypass patient eligibility denials. Our services ensure a hassle-free experience for both the providers and their patients. We ensure comprehensive eligibility checks through automation tech prior to services rendered. Through our system, the provider is immediately informed of pending patient responsibilities, Co-Pay, and other dues. We provide an aggressive check system where all patient’s statuses are verified.




