Let us convert your every denied claim into dollars. Consult with the best Denial Management Team

Implementing the best practices and streamlining the Process
In the long run, proper denial management in medical billing helps ensure the practice’s financial viability. A practise can raise collection rates and revenue while improving patient satisfaction by managing claim denials efficiently. These fundamentals should be considered by healthcare practises for effective denial management.:
- Prevention – Preventive actions can minimize denials. Implement these actions during pre-admission, registration, scheduling, and billing. However, denial management experts should oversee the progress and deliver information about the changes and the process from time to time.
- Analysis – When denials occur, analyze them to understand the cause and prevent them from reoccurring.
- Tracking Successful denial management in healthcare involves monitoring claim payment patterns and creating a system to pinpoint any deviation. It is crucial to determine the reasons for denials and enhance efficiency while reducing revenue losses.
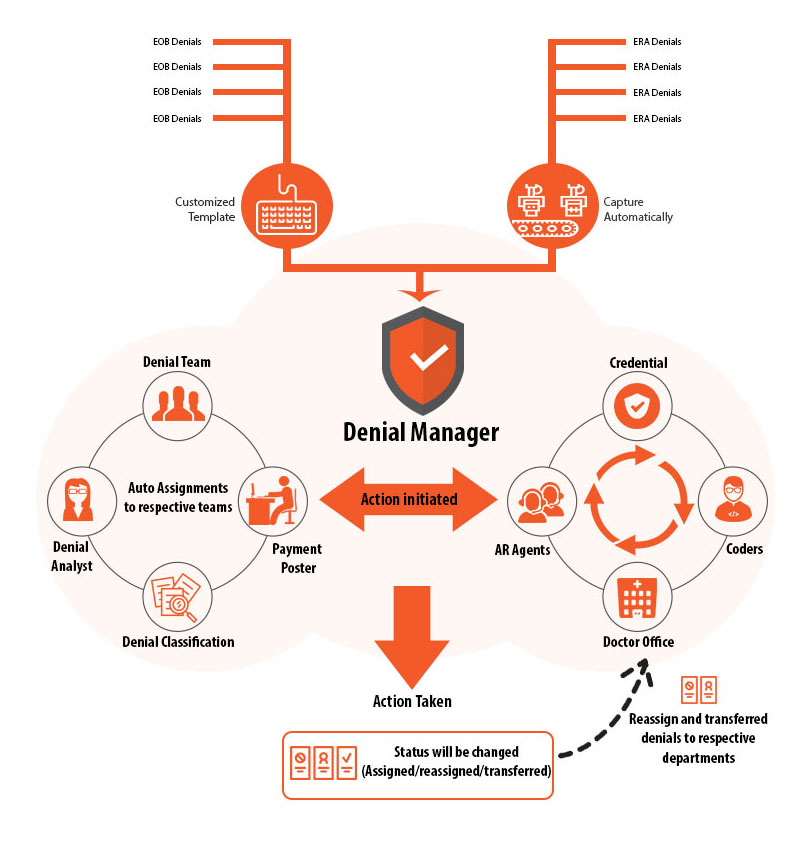
New technologies, tools, and software solutions are available to help healthcare practices oversee denials and take immediate action when they happen. Denial management in medical billing could implement an organized system for tracking denied claims. Another option is to outsource their revenue cycle management to specialists specializing in denial management in healthcare. That way, they can get a full suite of RCM management services that can boost the health of their revenue.





